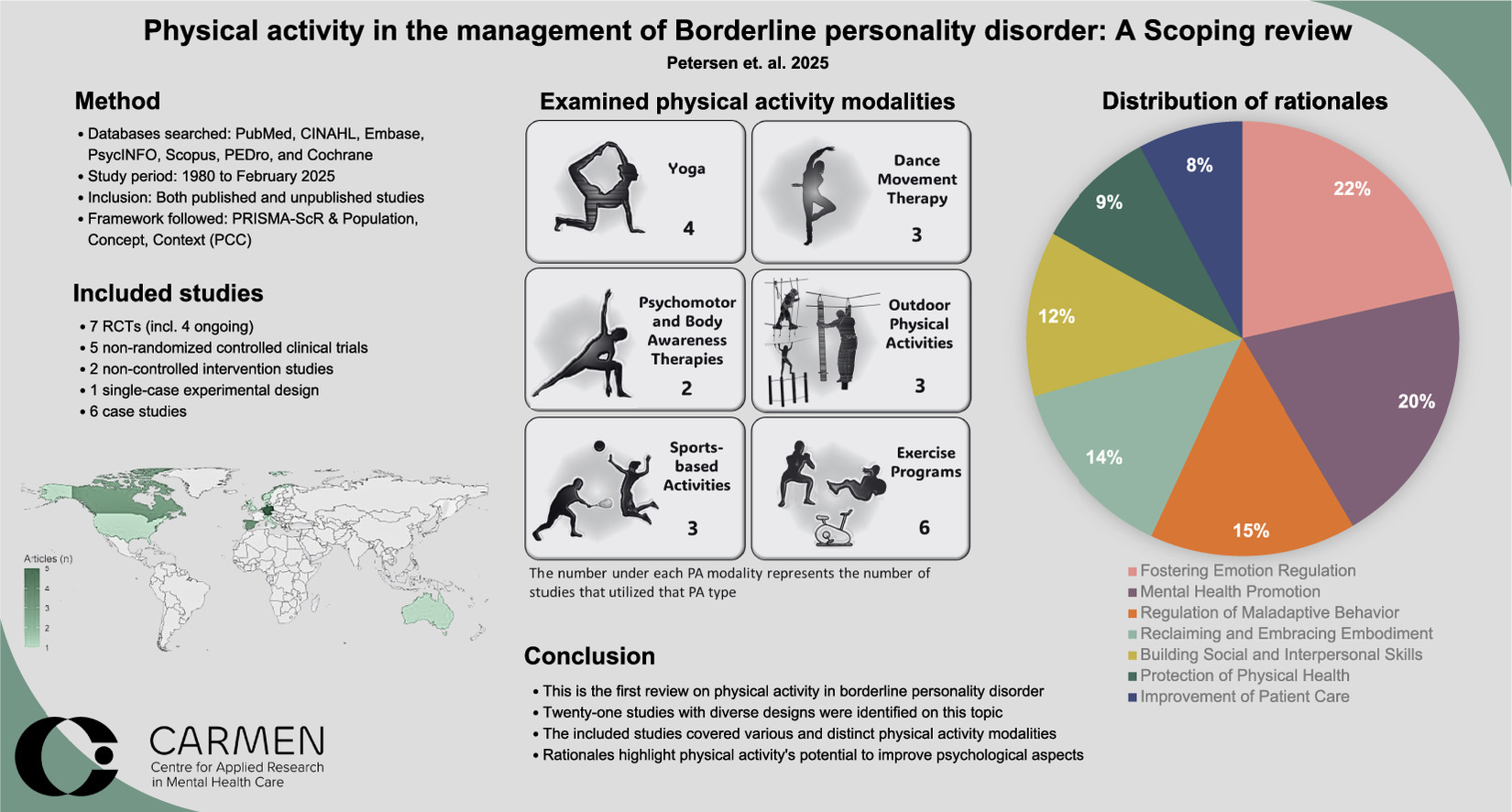
Author: Justine Petersen, PhD student, et al.
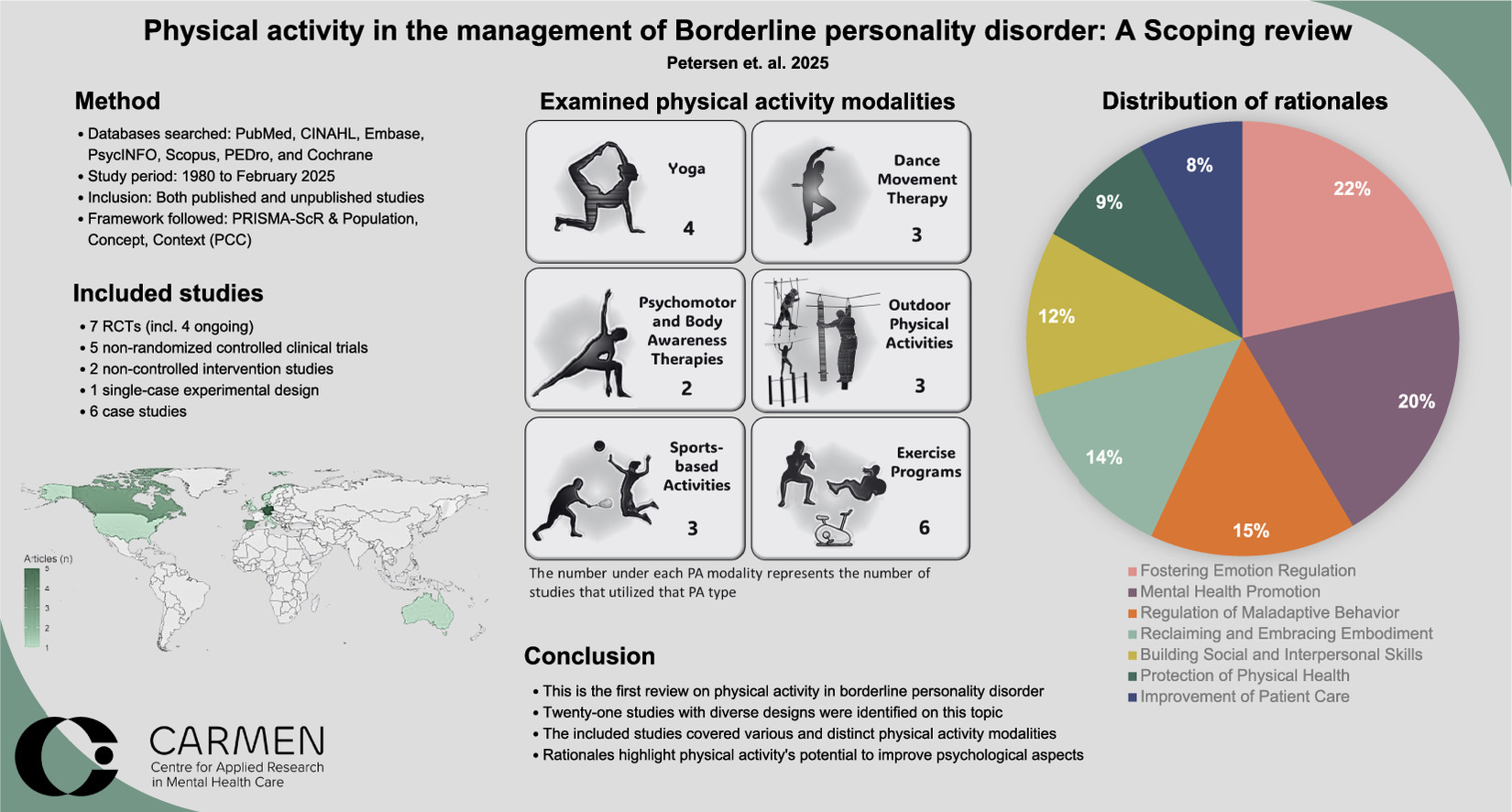
Abstract: In this the first review on physical activity in borderline personality disorder, 21 studies were reviewed covering various and distinct physical activity modalities. Rationales highlight physical activity’s potential to improve psychological aspects.
People with borderline personality disorder—affecting 1-2% of the US population and up to 20% of individuals undergoing mental health treatment —face a reduced life expectancy of 14–27 years, primarily due to suicide and cardiovascular-related issues. The studies reviewed here included 229 participants, primarily female, and covered six physical activity modalities: structured exercise; yoga; dance movement therapy; outdoor modalities; sports; and body awareness and psychomotor therapies.
Rationales for incorporating physical activity were: improving patient care; fostering emotional regulation; promoting mental health; regulating maladaptive behaviors; enhancing social skills; protecting physical health; and reclaiming embodiment; as well as fostering emotional regulation, the most prominent.
1. Download: Download high-res image (271KB) or
2. Download full-size image
The current standard of care for individuals with borderline personality disorder primarily relies on specialized psychotherapies, such as dialectical behavior therapy and mentalization-based therapy. While effective, these interventions are resource-intensive, requiring specialized expertise and significant financial investment, say the authors. “Moreover, they are often hospital-based and time-limited, potentially limiting their capacity to promote social inclusion, improve daily functioning, and address somatic health risks. Considering the high prevalence of physical inactivity among individuals with borderline personality disorder there is a pressing need for targeted interventions that improve physical health outcomes and overall wellbeing.”
Regular physical activity is widely recognized as a cornerstone of health promotion, playing a vital role in preventing and managing various physical and mental health conditions, while also contributing to a reduction in overall mortality, according to earlier research quoted in the review.
Engaging in physical activity reduces the risk of cardiovascular diseases, metabolic syndrome, stroke, diabetes, and certain cancers through mechanisms such as improved weight management, enhanced insulin sensitivity, strengthened cardiovascular and bone health, reduced inflammation, and a bolstered immune system.
In populations with mental illness, physical activity has been shown to mitigate stress, anxiety, and depression, while also improving sleep quality in non-clinical populations. Furthermore, research on the psychological effects of physical activity has demonstrated improvements in emotion regulation by decreasing negative affect and enhancing positive cognitive processes, thereby supporting overall wellbeing and quality of life. Evidence also supports the role of physical activity in alleviating symptoms and enhancing health outcomes in conditions such as major depressive disorder, anxiety disorders, PTSD and schizophrenia.
Conversely, say the authors, the use of physical activity in managing borderline personality disorder remains an underexplored and fragmented field.
Importance: This review highlights the promising but fragmented research on physical activity interventions for borderline personality disorder, with a primary emphasis on psychological aspects. Notable gaps include limited attention to somatic comorbidities and the lack of consistent outcome measures.
Availability: Published by Psychiatry Research.